Treating
AML with
VENCLEXTA +
decitabine
Actor portrayal.
Remission may be possible with VENCLEXTA + decitabine
VENCLEXTA + decitabine was studied in 13 adults with newly diagnosed AML who were age 75 years or older, or who had other medical conditions that prevented the use of standard chemotherapy. The clinical study did not include patients on decitabine alone.
Many people achieved some level of remission with VENCLEXTA + decitabine.
Percentage of patients achieving complete remission (CR) and complete remission with partial hematologic recovery (CRh)
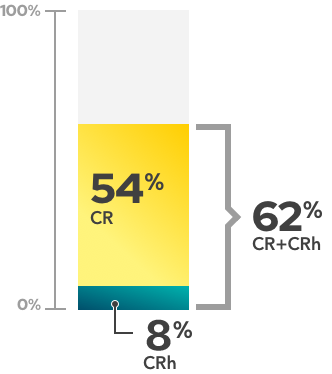
VENCLEXTA may not work for everyone.
When treated with VENCLEXTA + decitabine
- 54% (7 of 13 people) achieved complete remission (CR)
- 8% (1 of 13 people) achieved complete remission with partial hematologic recovery (CRh)
- 62% (8 of 13 people) achieved complete remission (CR) or complete remission with partial hematologic recovery (CRh)
How long does remission last?
Patients in the study were followed for a median of 11 months, with a range of 0.7 month to up to 38.8 months. The median length of time spent in complete remission (CR) was 13 months and in complete remission (CR) + complete remission with partial hematologic recovery (CRh) was 13 months.
VENCLEXTA can cause serious side effects, including tumor lysis syndrome, low white blood cell count, and infections. These are not all of the possible side effects of VENCLEXTA. Talk to your healthcare provider for more information about the risks and side effects of VENCLEXTA. Please see additional important safety information below.
Median means the middle number in a group of numbers that are arranged from lowest to highest. For example, in the group of numbers 1 to 13, 7 is the median.
Remission means a decrease in or disappearance of signs and symptoms of cancer.
CR, or complete remission, means the blood count is normal, fewer than 5% of bone marrow cells are leukemia cells, and there are no signs or symptoms of leukemia elsewhere in the body. When there is CR:
- Patients do not need to receive red blood cell transfusions
- Patients may not need to receive platelet transfusions based on their platelet levels and no signs of bleeding
CRh, or complete remission with partial hematologic recovery, means that some remission has occurred. When there is CRh, no signs of cancer are seen, but some blood counts have not returned to normal levels.
Actor portrayal.
Side effects may occur with VENCLEXTA + decitabine.
How long does it take for patients to respond to treatment?
In the clinical study, the median time for patients to achieve some level of remission for either CR or CRh was 2 months (with a range of 0.8 to 4.2 months). Remember, VENCLEXTA works differently for everyone. The time it takes to work and how long the effects last may vary from person to person.
Median means the middle number in a group of numbers that are arranged from lowest to highest. For example, in the group of numbers 1 to 13, 7 is the median.